The purpose of APOS Fellow status is to recognize and honor outstanding contributions to the science and practice of psychosocial oncology. Membership in the Fellowship is not purely honorific, however: it carries an expectation of ongoing contributions to and leadership within the Society.

Are you interested in becoming an APOS Fellow? We invite nominations!
APOS is honored to support those who contribute to our ever-evolving field. Our previous classes of APOS Fellows are a testament to the history of our organization. Learn more about them below
Past Fellows
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2023

Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
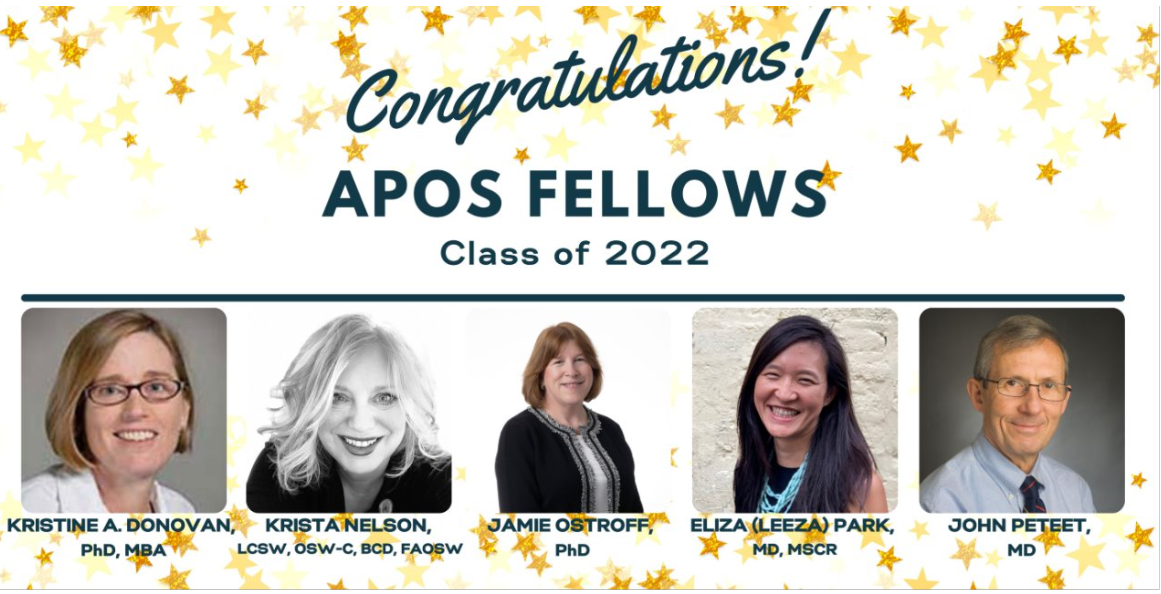
Class of 2022
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2021
 Dr. Scott A. Irwin is currently the Director of Cedars-Sinai Cancer’s Patient and Family Support Program and a Professor of Psychiatry and Behavioral Neurosciences within Cedars-Sinai Health System. His career focuses on improving outcomes for those with cancer or other progressive, potentially life-limiting illnesses, and their families, through leading-edge clinical services, ongoing research, and program development, improvement, and implementation. He is widely published, has been recognized at many levels for his research, teaching, consulting, and clinical endeavors, and has received research funding from the NCI, NIMH, the National Palliative Care Research Center, the Archstone Foundation, and industry.
Dr. Scott A. Irwin is currently the Director of Cedars-Sinai Cancer’s Patient and Family Support Program and a Professor of Psychiatry and Behavioral Neurosciences within Cedars-Sinai Health System. His career focuses on improving outcomes for those with cancer or other progressive, potentially life-limiting illnesses, and their families, through leading-edge clinical services, ongoing research, and program development, improvement, and implementation. He is widely published, has been recognized at many levels for his research, teaching, consulting, and clinical endeavors, and has received research funding from the NCI, NIMH, the National Palliative Care Research Center, the Archstone Foundation, and industry.
Dr. Irwin earned his Bachelor of Science from the University of California, Los Angeles, and both his MD and PhD (neuroscience) at the University of Illinois, Urbana-Champaign. He successfully completed his psychiatry residency at UC San Diego as chief resident of Outpatient Psychiatric Services, as well as a two-year elective in hospice and palliative care at San Diego Hospice and The Institute for Palliative Medicine. He is a diplomate of the American Board of Psychiatry and Neurology, with subspecialty certification in psychosomatic medicine.
 Dr. Lynne Padgett is a rehabilitation psychologist who has worked in multiple healthcare and cancer care settings, including the School of Medicine at Emory University, Kaiser Permanente Department of Hospital Medicine, the National Cancer Institute, the American Cancer Society, and currently at the Washington, D.C. Veterans Affairs Medical Center. Her research interests are at the intersections of cancer rehabilitation, psychosocial and palliative care in oncology. More specifically she has worked in screening for distress, symptoms and physical function in cancer patients, palliative care decision making, cognitive and psychosocial effects of cancer and cancer treatment and the implementation of evidenced based care in community cancer settings.
Dr. Lynne Padgett is a rehabilitation psychologist who has worked in multiple healthcare and cancer care settings, including the School of Medicine at Emory University, Kaiser Permanente Department of Hospital Medicine, the National Cancer Institute, the American Cancer Society, and currently at the Washington, D.C. Veterans Affairs Medical Center. Her research interests are at the intersections of cancer rehabilitation, psychosocial and palliative care in oncology. More specifically she has worked in screening for distress, symptoms and physical function in cancer patients, palliative care decision making, cognitive and psychosocial effects of cancer and cancer treatment and the implementation of evidenced based care in community cancer settings.
She is interested in the potential of technology to extend the reach of clinical care and to facilitate screening and referrals. Her clinical work focuses on symptom management in cancer patients, particularly cognition and fatigue. She has published in these areas and works as part of two writing and research teams.
Dr. Padgett currently serves as the APOS Secretary and served as Director of Research. She is also a member of the American Congress of Rehabilitation Medicine, where she is a member of the Cancer Rehabilitation Cognition and Research and Outcomes working groups. Dr. Padgett’s work has been characterized by a focus on translation scientific evidence into care. From her experiences she has taken the following lessons: If it’s worth doing, it’s worth evaluating; Quality care builds on the unique strengths of a cancer center; and Start programs where they are excited to see you!
 Dr. Jon Levenson‘s specialty within psychiatry includes consultation-liaison psychiatry. He is boarded in the related subspecialty of Psychosomatic Medicine. Within these fields Dr. Levenson's special areas of interest include psychiatric aspects of AIDS and Oncology, as well as psychiatric contributions to palliative care. He is past president of both the American Psychosocial Oncology Society and the Society for Liaison Psychiatry. Dr. Levenson is also interested in the training of medical students, residents, as well as other health professionals in the psychiatric aspects of medicine.
Dr. Jon Levenson‘s specialty within psychiatry includes consultation-liaison psychiatry. He is boarded in the related subspecialty of Psychosomatic Medicine. Within these fields Dr. Levenson's special areas of interest include psychiatric aspects of AIDS and Oncology, as well as psychiatric contributions to palliative care. He is past president of both the American Psychosocial Oncology Society and the Society for Liaison Psychiatry. Dr. Levenson is also interested in the training of medical students, residents, as well as other health professionals in the psychiatric aspects of medicine.
 Dr. Elyse Park is a clinical health psychologist and health services researcher who focuses on improving health-related behaviors among populations at risk for cancer and survivors. Her research is conducted at the MGH Mongan Institute for Health Policy and she co-directs the cancer survivorship program at the MGH Cancer Center. Additionally, she is director of Behavioral Research at the Benson-Henry Institute for Mind Body Medicine at MGH and the MGH Tobacco Research and Treatment Center.
Dr. Elyse Park is a clinical health psychologist and health services researcher who focuses on improving health-related behaviors among populations at risk for cancer and survivors. Her research is conducted at the MGH Mongan Institute for Health Policy and she co-directs the cancer survivorship program at the MGH Cancer Center. Additionally, she is director of Behavioral Research at the Benson-Henry Institute for Mind Body Medicine at MGH and the MGH Tobacco Research and Treatment Center.
Her research focuses on developing and implementing behavioral interventions to enhance resiliency, decrease tobacco use, and improve access to healthcare. She founded the MGH Qualitative Mixed Methods Research Unit. She has been funded by the American Cancer Society (ACS), the National Cancer Institute (NCI), the Robert Wood Johnson Foundation (RWJ), and the Livestrong Foundation to support her survivorship and cancer prevention research. Her contributions are reflected in 250 peer-reviewed publications. Clinically, she treats cancer survivors. She founded two hospital-based clinical services: the MGH Cancer Center’s Smokefree Support Service and the MGH Cancer Center Resiliency Survivorship Group Program.
 Dr. Alla Sikorskii is a Professor in the Department of Psychiatry, College of Osteopathic Medicine, Michigan State University. Dr. Sikorskii has formal training in Statistics and Probability and a track record of successful productive collaboration with health researchers and clinicians. She has built a program of research in cancer symptom management and patient-reported outcomes, and design and evaluation of interventions to improve these outcomes among people with cancer and other chronic conditions.
Dr. Alla Sikorskii is a Professor in the Department of Psychiatry, College of Osteopathic Medicine, Michigan State University. Dr. Sikorskii has formal training in Statistics and Probability and a track record of successful productive collaboration with health researchers and clinicians. She has built a program of research in cancer symptom management and patient-reported outcomes, and design and evaluation of interventions to improve these outcomes among people with cancer and other chronic conditions.
Dr. Sikorskii has designed numerous randomized controlled trials (RCTs) including procedures for screening, randomization, timing of longitudinal assessments, measurement of important factors, and ways to control for them. Her completed work includes defining the cut-points for symptom severity and anchor-based definition of responses to multiple cancer-related symptoms, in collaboration with Drs. Barbara and Charles Given. She has proposed and successfully implemented the innovative analyses of response and times to response to the management of multiple symptoms. She has served as a co-investigator and statistician on 18 NIH-funded R01 grant projects. Her most recent work is devoted to the advance from traditional RCTs that test fixed interventions to adaptive interventions tailored to individuals. This shift requires research that sequences interventions and creates decision rules for switching from one intervention to another based individuals’ demonstrated needs. When an intervention does not initially work, clinical logic is to either extend the timeframe or move to a more intensive intervention. This logic leads to multi-staged interventions, where the subsequent stage is individually tailored, based on the response to the previous intervention (stage). The sequential multiple assignment randomized trial (SMART) allows to build the evidence base for multi-staged interventions. Dr. Sikorskii has led the applications of the SMART design to test sequences of supportive care interventions among people with cancer.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2020
 KAREN KAYSER, MSW, PHD
KAREN KAYSER, MSW, PHD
Dr. Karen Kayser holds the Dr. LaRocca Chair in Oncology Social Work at the University of Louisville, Kent School of Social Work. She earned in interdisciplinary PhD in Social Work and Psychology from the University of Michigan. Upon completing her PhD, she worked as an NICHD Post-doctoral Fellow on a clinical research with families coping with childhood cancer. This experience inspired her to pursue her career in psychosocial oncology with a particular focus on studying cancer within the context of families and intimate relationships.
After her post-doc, Dr. Kayser was offered an Assistant Professor position at the Graduate School of Social Work at Boston College where she taught and conducted research for the next 20 years. During her years in Boston, her research agenda focused on studying the interpersonal and cultural factors that impact adjustment to cancer. She developed a couple-based intervention for breast cancer patients (Partners in Coping) and conducted a randomized controlled trial at Dana-Farber Cancer Institute and Massachusetts General Hospital. She disseminated the Partners in Coping treatment protocol in the book Helping Couples Cope with Women’s Cancers: An evidence-based approach for practitioners (co-authored with Dr. Jennifer Scott; Springer, 2008).
In 2011, Dr. Kayser left Boston College to become the inaugural Endowed Chair in Oncology Social Work at the University of Louisville (UofL). As the Dr. LaRocca Chair, she has developed innovative educational and research programs with the goal of building the workforce capacity to provide evidence-based psychosocial oncology services. Nationally, she established the first program in Psychosocial Oncology in a graduate school of social work. Her clinical research has focused on improving the delivery of distress screening and management services in cancer care. She collaborated with Dr. Brad Zebrack and the Association of Oncology Social Work on A Project to Assure Quality Cancer Care (APAQCC) and the Patient-Centered Research Collaborative (PCRC). Her current research focuses on the promotion of cervical cancer screening and the HPV vaccination in rural Kentucky where rates of HPV-related cancers are among the highest in the nation. Dr. Kayser also serves as the Editor-in-Chief of the Journal of Psychosocial Oncology.
 ANNA (NINA) MURIEL, MD, MPH
ANNA (NINA) MURIEL, MD, MPH
Dr. Anna (Nina) Muriel is a Child Psychiatrist and Chief of the Division of Pediatric Psychosocial Oncology at the Dana-Farber Cancer Institute (DFCI). After Adult and Child Psychiatry training at Massachusetts General and McLean Hospitals, she worked in the Marjorie E. Korff Parenting at a Challenging Time Program at MGH providing care to adults with cancer and their families. She developed the Parenting Concerns Questionnaire to measure the concerns of parents with cancer and co-authored the book “Raising an Emotionally Healthy Child When a Parent is Sick.”
Her more recent work has been in Pediatric Psycho-social Oncology leading a multi-disciplinary clinical team at DFCI and participating in the development of the National Standards of Psychosocial Care for Children with Cancer. She has also explored the intersection between psychiatry and palliative care and psychopharmacology in pediatric oncology. She is Assistant Professor of Psychiatry at Harvard Medical School, and co-edited “Pediatric Psychosocial Oncology: Textbook for Multidisciplinary Care.”
 CRISTINA POZO-KADERMAN, PHD
CRISTINA POZO-KADERMAN, PHD
Cristina Pozo-Kaderman, Ph.D. is the Director of Clinical Operations for Cancer Support Services at Sylvester Cancer Center and Voluntary Faculty in the Department of Psychiatry and Behavioral Sciences at the University of Miami for the past 3 years. She obtained her doctorate in clinical psychology from the University of Miami. She completed her internship at Cornell Medical College, Payne Whitney Clinic and her fellowship in psycho-oncology at Memorial Sloan Kettering Cancer Center. She was at the Mount Sinai Cancer Center on Miami Beach for 22 years. She is a clinical psychologist & certified in sex therapist for oncology patients.
During graduate school she was awarded the Patricia Roberts Harris fellowship for minorities and women which provided support for her doctoral training and allowed her to develop her own research study for her Master’s and doctoral dissertation. She designed a longitudinal study following women from diagnosis to one year post treatment and women were assessed at 5 time periods with a combination of interview and standardized measures looking at coping strategies, social support, and marital satisfaction. This research study served a pilot project for grant application and award from ACS to look at how minority women adjust to a breast cancer diagnosis.
Dr. Pozo-Kaderman’s dream came true when she was accepted to MSKCC fellowship in psycho-oncology and she had the opportunity to work with Jimmie Holland, Paul Jacobsen, Steve Passik, Bill Redd, Lynna Lesko, and Bill Breitbart.
After returning from MSKCC, Dr. Pozo-Kaderman spent a year at the Sylvester Cancer Center as faculty in Psychiatry and helped establish the first psycho-oncology program at Sylvester. She was then offered the opportunity to create and develop the psychosocial program for south Florida for Salick Healthcare, which strongly supported psychosocial services (social work, psychological, psychiatric, nutritional, and palliative) being offered to all cancer patients and families. Her career at this point shifted and became more clinical care and administrative, but she continued to supervise clinically for a year-long practicum doctoral students from the University of Miami clinical health program, lecture on psychosocial oncology, and serve on dissertation committees. She has been actively involved in the community making presentations on psychosocial oncology issues, actively involved in Komen Kids, was on the founding board for the Cancer Support Community in Miami, and serve(s) as a local resource while keeping a busy clinical psycho-oncology practice and seeing oncology sex therapy cases. Most recently Dr. Pozo-Kaderman has been back at the University of Miami, Sylvester Cancer Center where she has administratively worked to develop and grow across the main campus and 7 satellites Cancer Support Services where patients receive free of charge music and art therapy, massage, exercise physiology, yoga, pet therapy, chaplaincy and spiritual counseling, patient resource centers, and volunteers. In addition she oversees services requiring insurance such psychology, psychiatry, and acupuncture, while continuing to clinically see patients and supervise psychology doctoral students. She has now developed a year-long program for nurses to help cope with compassion fatigue. She continues to be actively involved in community programs.
 SHARLA WELLS-DI GREGORIO, PHD
SHARLA WELLS-DI GREGORIO, PHD
Sharla Wells-Di Gregorio is an Assistant Professor of Internal Medicine, Division of Palliative Medicine at The Ohio State Wexner Medical Center Arthur G. James Cancer Hospital where she provides clinical psychology services for Psychosocial Oncology and Palliative Medicine. Dr. Wells-Di Gregorio completed her Ph.D. in clinical psychology at Northwestern University Medical School, a pre-doctoral internship at UCLA, and a postdoctoral fellowship in Biobehavioral Oncology at Ohio State. Her early research focused on the psychological and immune impact of caregiver stress for men whose wives had recurrent breast cancer. In 2005, she began her position with the palliative medicine team at OSU where she works primarily with patients and families with advanced cancer and at the end of life. Her research focuses on translation and empirical validation of psychological multi-symptom interventions, evaluation of psychosocial oncology models of care, and studies to improve oncology communication, particularly for patients with serious illness. In her role at Ohio State, she developed a two-year Psychosocial Oncology & Palliative Medicine Fellowship Program to train clinical psychologists to provide evidence-based psychological and symptom management care for cancer patients. She chaired the multi-disciplinary committee at the James Cancer Hospital to validate a distress measure, the James Supportive Care Screening, to identify patients’ most common and distressing comprehensive oncology concerns and connect them with Supportive Care Services. She has served as Director of Professional Education for the American Psychosocial Oncology Society (2017-2022) for which she oversees a national committee of 20 individuals responsible for the education and training of psychologists, nurses, psychiatrists, and social workers. The current focus of this committee’s work is creation and assessment of an Online Psychosocial Oncology Core Curriculum and establishment of productivity benchmarks for the field of psychosocial oncology.
 GWEN WYATT, PHD, RN
GWEN WYATT, PHD, RN
Over the past 30+ years Dr. Gwen Wyatt pursued psychosocial oncology with a continuously funded program of research. She is a full professor in the College of Nursing at Michigan State University (MSU). Her research focuses on reducing symptoms and improving the quality of life of cancer patients, and, more recently, their informal caregivers. She has served as PI on nine completed studies focusing on psychosocial oncology. Specific interest areas include end of life care, integrative therapies and the economics of incorporating integrative therapies into mainstream health care. Her research of complementary therapies have evaluated acupressure, meditation, imagery, therapeutic touch, reminiscence therapy and reflexology. Her nurse-designed interventions for symptom management in the home address the shift in care from hospital to clinic to home. Findings from her work on supportive cancer care have been consistently disseminated nationally and internationally through publications and presentations.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2019
 Vicki Kennedy, LCSW
Vicki Kennedy, LCSW
Vicki Kennedy, LCSW is the Executive Director of Oncology Strategy and Patient Engagement for Cullari Communications Global. Ms. Kennedy is leading expert in psychosocial oncology including screening and management of cancer-related distress, treatment decision support, and effective integration of patient engagement strategies that help define patient value, improve quality of life and enhance health outcomes. Prior to coming to CCG, Vicki served as Vice President of Program Development & Delivery for the Cancer Support Community (CSC) in Washington, DC, where she was responsible for development, delivery and quality assurance of CSC clinical programs worldwide. An oncology social worker for the past 35 years, Ms. Kennedy has dedicated her career to ensuring that people touched by cancer have awareness of and access to evidence-based psychosocial care. Vicki is a past-president of Association of Oncology Social Work and currently serves on the board of the American Psychosocial Oncology Society. She also serves on the Editorial Board for the Journal of Oncology Practice Management. A leading speaker for patient advocacy, engagement and survivorship, Ms. Kennedy was awarded the Association of Oncology Social Work’s Quality of Life in Cancer Care Award highlighting oncology social work’s commitment to improving the lives of people with cancer.
 Donald L. Rosenstein, MD
Donald L. Rosenstein, MD
Dr. Rosenstein is Professor of Psychiatry and Medicine at the University of North Carolina where he is Director of the Comprehensive Cancer Support Program and Vice-Chair of the Division of Hospital Psychiatry. Dr. Rosenstein earned his undergraduate degree in psychology from Wesleyan University, his medical degree from Northwestern University School of Medicine, and completed his residency training in psychiatry at Yale University. He is the former Clinical Director of the National Institute of Mental Health (NIMH) and Past-President of both the Academy of Consultation Liaison Psychiatry and the American Psychosocial Oncology Society (APOS). Dr. Rosenstein and Justin Yopp, PhD are the authors of The Group: Seven Widowed Fathers Reimagine Life (Oxford University Press).
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2018
 Joseph Greer, PhD
Joseph Greer, PhD
Dr. Joseph Greer is the Program Director of the Center for Psychiatric Oncology & Behavioral Sciences and the Associate Director of the Cancer Outcomes Research Program at the Massachusetts General Hospital Cancer Center. He is also an Assistant Professor of Psychology at Harvard Medical School.
Dr. Greer's research focuses on the development and testing of supportive care interventions for patients with cancer. As the principal investigator and collaborator on numerous grant-funded projects, he is studying the application of cognitive-behavioral therapy (CBT) to treat anxiety in patients with advanced cancer; nurse-delivered behavioral interventions to improve breathlessness in patients with lung cancer; the use of mobile technology to promote symptom management and adherence to oral chemotherapy medications; and the benefits of early palliative care integrated with standard oncology care. Dr. Greer has published over 85 scholarly papers, reviews, chapters, and commentaries related to this work. He has received funding from the National Institutes of Health, American Cancer Society, Patient Centered Outcomes Research Institute, and philanthropic donations. Dr. Greer’s program of research is greatly informed by his clinical practice at the MGH Cancer Center where he provides CBT for patients and their families.
 Isabel Schuermeyer, MD
Isabel Schuermeyer, MD
Dr. Schuermeyer is a psychiatrist who is board certified in Consultation-Liaison psychiatry (previously psychosomatic medicine) and has worked at the Cleveland Clinic since completing fellowship in 2005. While in fellowship she started working in the field of Psychosocial Oncology and helped develop the Interdisciplinary Psychosocial Oncology team at the Taussig Cancer Center.
Dr. Schuermeyer is a clinician who treats patients with cancer along with either new onset psychiatric symptoms or exacerbation of an underlying psychiatric illness. Her focus has been on a team-based approach, including the oncology team, given the risk of interactions between psychiatric medicines and cancer treatments. Her research interests are end of life decisions, determining capacity and working within an interdisciplinary team. She is a past-president of American Psychosocial Oncology Society and has been involved with the American Psychiatric Association.
Dr. Schuermeyer is active in teaching psychiatry residents and fellows, as well as palliative medicine fellows. When not at work, she is busy being a soccer mom, talking her husband out of buying a truck to haul more beehives, making soap, and attempting to keep her kids out of trouble.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2017
 Barry Bultz, PhD
Barry Bultz, PhD
Dr. Bultz is Professor and Head of the Division of Psychosocial Oncology, and holds The Daniel Family Leadership Chair in Psychosocial Oncology at the Cumming School of Medicine, University of Calgary. He is also Professor of Psychiatry in the Cumming School of Medicine. He is also the Director of the multidisciplinary Department of Psychosocial Oncology at the Tom Baker Cancer Centre.
Dr. Barry Bultz is an active member of many collaborative research initiatives, holds several grants and has published over 100 papers. He serves on a number of editorial boards for cancer-related journals. Dr. Bultz carries the message of the importance of attention to the emotional needs of the patient into many areas in the health care system. He advocates for the importance of recognizing the impact of cancer related distress on the patient’s experience. He has championed, advocated, published and presents frequently on the importance of Screening for Distress and has promoted “Distress” being branded the “6th Vital Sign.”
Dr. Bultz is a co-founder and Past President of the Canadian Association of Psychosocial Oncology (CAPO). From 2003 to 2006, Dr Bultz served as an Invited Director of the Board of the American Psychosocial Oncology Society. From 2012 to 2014, Dr. Bultz served as President of the International Psycho-Oncology Society. He is a Fellow of the Canadian Psychological Association. He received the Award of Excellence in Medicine and Health from the Canadian Cancer Society
– Alberta Division, and the Award of Excellence from the Canadian Association of Psychosocial Oncology. In 2016 he was the recipient of the Arthur M. Sutherland Award from the International Psycho-Oncology Society. In 2016, he also was honoured with the Alberta Order of Excellence, the Province’s highest honour bestowed upon Albertans who have served with excellence and distinction and whose contributions have made a lasting impact.
 Michelle Fingeret, PhD
Michelle Fingeret, PhD
Dr. Michelle Fingeret initiated her psychosocial oncology career following the acquisition of her PhD in Clinical Psychology from the University of Texas A&M in 2004. In 2007, she was appointed as Assistant Professor within the MD Anderson Cancer Center in the Department of Behavioral Science with in the Division of Cancer Population Sciences, and later promoted to Associate Professor in 2013. Also, Dr. Fingeret received additional appointments as an Assistant Professor in 2007 in the Departments of Head & Neck Surgery and Plastic Surgery, and as Associate Professor in 2013.
Dr. Fingeret’s research background and clinical expertise are in the areas of body image, psychosocial oncology, and quality of life for cancer survivors. The multidisciplinary research she has been conducted includes both small and large research studies, many of which have been funded through institutional grants, the National Institutes of Health, and the American Cancer Society. Much of her work involves collaborating with investigators across the United States in various fields such as surgical oncology, reconstructive surgery, and biomedical engineering. Her research is centered on identifying the nature and extent of body image concerns in different cancer populations, identifying risk factors associated with poor psychological adjustment to alterations in body image, and developing psychotherapeutic interventions to alleviate body image suffering in the oncology setting. In addition to her research activities, she is the founder and director of the Body Image Therapy Service. This unique program provides psychological counseling to patients experiencing distress related to body image changes resulting from cancer treatment at MD Anderson Cancer Center.
Dr. Fingeret has been a co-author on 42 peer-reviewed original research articles, 4 invited articles, 5 book chapters, and 10 published abstracts. In terms of conference presentations, she has presented at 4 symposia, 5 invited workshops, and more than 50 scientific exhibitions. Equally impressive, Dr. Fingeret has made a serious commitment to teaching courses within her institution, training programs, mentoring initiatives, and clinical and teaching supervision.
As for APOS, she has been a member of the Annual Scientific Program Committee since 2009, Marketing Chair from 2010-2011, Treasurer from 2011-2012, and President Elect/President/Past President from 2013-present. Dr. Fingeret helped to develop and launch the APOS Webinar Series as well as the APOS Future Fund. As President, she presided over the APOS/IPOS World Congress of Psycho- Oncology. During these past three years, she also carefully steered APOS through a difficult transition of identifying a new management firm without disruptions to APOS’ daily operations.
 Barbara Given, PhD, RN, FAAN
Barbara Given, PhD, RN, FAAN
Dr. Barbara Given is one of the most consistently well-funded nursing researchers in oncology nursing. She has successfully obtained funding from the National Institutes for Health for more than 30 years. Her areas of investigation include long- term cancer home care, family caregivers, cancer nursing intervention, adherence with oral cancer medication and cancer symptom management. Her research has employed Interactive Voice Response systems to monitor symptoms of patients in their homes, and to provide them with evidence- based information to manage their symptoms using a Symptom Management Toolkit her team developed.
She is one of the charter members of the Midwest Nursing Research Society and the Oncology Nursing Society. She was honored at Michigan State University as a University Distinguished Professor (2001), was the Associate Dean for Research College of Nursing (2007-2012) and Director of the PhD program College of Nursing (2007-5/2015). She is currently the Interim Associate Dean for Research and the PhD Program. She serves on the Sparrow Health System Governing Board where she is the Chair. She is a Visiting Professor at Vanderbilt.
Honors include: the Council for the Advancement of Nursing Science (CANS) Outstanding Nurse Scientist Award (2016), Burdette Kunkel Behavioral Research Achievement Award, presented by the Behavioral Cooperative Oncology Group (2014), Distinguished Oncology Nursing Lectureship from the James Cancer Hospital at The Ohio State University Comprehensive Cancer Center (2013), Sparrow Nurses Lifetime Achievement Award (2013), ONS Distinguished Service Award (2006), Oncology Nursing Society (ONS)/Schering Excellence in Cancer Nursing Research Award (2002), Friends of the National Institute for Nursing Research Pathfinder Distinguished Researcher Award (2001), the Lifetime Achievement Award from the MSU College of Nursing Alumni Association (2000), The Cancer Nursing’s Research Article Award was named in her honor (2013). She began her work with Sparrow Hospital in January 1966.
 Cecile Lengacher, PhD, RN, FAAN
Cecile Lengacher, PhD, RN, FAAN
Dr. Cecile Lengacher is an internationally recognized nurse scientist, with expertise in bio-behavioral clinical trial intervention research including psycho-oncology, psychoneuroimmunology, and complementary alternative medicine (CAM), emphasizing the link between physiological and behavioral outcomes for cancer survivors. She is a Professor and Director of the Pre-Doctoral Fellowship Program at the USF College of Nursing and for the past 19 years serves as a faculty member of the Moffitt Cancer Center Outcomes and Behavioral Program in the Population Sciences Division, and Integrative Medicine, and Breast Cancer Clinical Programs.
Nationally, she is honored as a Fellow of the American Academy of Nursing and has participated as a member of the NIH BMIO Scientific Review Study Section, along with being a reviewer for several journals including Psycho-Oncology. She has extensive experience in leading bio-behavioral multidisciplinary teams to test the efficacy of MBSR on psychological, physical, and biological outcomes among cancer survivors and caregivers for multiple NCI and other funded grants. She has published over 120 peer-reviewed papers published in peer-reviewed journals, including Psycho-Oncology, and numerous book chapters, monographs, and technical reports that include the effects of CAM therapy intervention research on symptoms and quality of life while examining the biological mechanisms of action, natural killer cells, stress hormones, cytokines, telomeres, and genes.
Her research has advanced the scientific evidence of behavioral intervention research and symptom science to improve the quality of life among cancer survivors and caregivers. She has clearly made significant contributions to the science of psychosocial oncology by presenting her research findings internationally at IPOS annual meetings and at every APOS scientific meeting since 2005. For a decade she has been a member of the APOS Scientific Review Committee; she has also served on the Program Committee and as Co-Chair of the IPOS/APOS 2015 Scientific Review Committee, along with serving on the Research committee and Secretary of the APOS Board since 2015.
 Maryland Pao, MD
Maryland Pao, MD
Dr. Maryland Pao is the Clinical Director and Deputy Scientific Director of the National Institutes of Health Intramural Research Program at the National Institutes of Health. She serves as Chief of the Psychiatry Consultation Liaison Service in the Hatfield Clinical Research Center. A native of Bethesda, she attended Wellesley College before completing a BA/MD program at Johns Hopkins University School of Medicine. She completed Pediatric and Psychiatric Residency training as well as a Child and Adolescent Psychiatry Fellowship at Johns Hopkins Hospital. Boarded in Pediatrics (1994, 2001), she is currently certified in General Psychiatry, Child and Adolescent Psychiatry and Psychosomatic Medicine.
Her research interests are in the complex interactions between medical and psychiatric symptoms in pediatric oncology, pediatric HIV and other primary immunodeficiencies and in the impact of these diseases on a person’s development. She studies distress and its correlates in medically ill children including suicidal thoughts and behaviors. She has published more than 120 research articles and chapters, and co-edited the Quick Reference for Pediatric Oncology Clinicians: The Psychiatric and Psychological Dimensions of Pediatric Cancer Symptom Management, 2nd edition, Oxford University Press, Oxford, 2015. She helped develop the ASQ™ (Ask Suicide-Screening Questions), a suicide screening tool for pediatric emergency departments, and Voicing My CHOiCES™, an advance care planning guide for adolescents and young adults.
Dr. Pao has been a member of APOS since 2008. A leader in promoting the field of pediatric psychosomatic medicine, she is a recipient of the 2012 AACAP Simon Wile Award for leadership in Consultation. She is on the Clinical Faculty at Georgetown University, George Washington University and at Johns Hopkins University Schools of Medicine.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2016
 Betty Ferrell, RN, PhD, MA, FAAN, FPCN, CHPN
Betty Ferrell, RN, PhD, MA, FAAN, FPCN, CHPN
Dr. Ferrell has been in nursing for 37 years and has focused her clinical expertise and research in pain management, quality of life, and palliative care. She is the Director of Nursing Research & Education and a Professor at the City of Hope Medical Center in Duarte, California. She is a Fellow of the American Academy of Nursing and she has over 370 publications in peer-reviewed journals and texts. She is Principal Investigator of a Research Project funded by the National Cancer Institute on “Palliative Care for Patients with Solid Tumors on Phase 1 Clinical Trials” and Principal Investigator of the “End-of-Life Nursing Education Consortium (ELNEC)” project. She directs several other funded projects related to palliative care in cancer centers and QOL issues. Dr. Ferrell is a member of the Board of Scientific Advisors of the National Cancer Institute and was Co-Chairperson of the National Consensus Project for Quality Palliative Care. Dr. Ferrell completed a Masters degree in Theology, Ethics and Culture from Claremont Graduate University in 2007. She has authored ten books including the Oxford Textbook of Palliative Nursing published by Oxford University Press (4th edition published in 2015). She is co-author of the text, The Nature of Suffering and the Goals of Nursing published in 2008 by Oxford University Press and Making Health Care Whole: Integrating Spirituality into Patient Care (Templeton Press, 2010). In 2013 Dr. Ferrell was named one of the 30 Visionaries in the field by the American Academy of Hospice and Palliative Medicine.
 Stewart B. Fleishman, MD
Stewart B. Fleishman, MD
Stewart B Fleishman, MD is the Founding Director of Cancer Supportive Services at Continuum Cancer Centers of New York: Beth Israel and St. Luke’s-Roosevelt, now part of the Mount Sinai Health System. While at Continuum, he also served as the Associate Chief Medical Officer of Continuum Jacob Perlow Hospice and its Ethics Committee Chair.
With the good fortune of serving as a Psycho-oncology Fellow at Memorial Sloan-Kettering Cancer Center under Dr. Jimme Holland’s mentorship, he has a varied medical career at the forefront of interdisciplinary cancer treatment. He served as Bioethics Committee Chair of a 13 hospital network at Long Island Jewish Medical Center (now part of Northwell Health), where he also developed its Psycho-oncology and Supportive Care Program.
Dr. Fleishman has been an investigator at the Cancer and Leukemia Group B (now the Alliance for Clinical Trials in Oncology) since 1986, and was the Vice Chair of its Quality of Life Sub-Committee. His research interests include quality of life assessment and trials to reverse cancer cachexia, fatigue, nausea and vomiting, testosterone loss in male patients, cognitive impairment in survivorship. He serves on the NCCN Distress Management Guidelines Committee. He is the author of the patient-friendly LEARN to Live Through Cancer: What You Need to Know and Do and the accompanying provider’s textbook Manual of Cancer Treatment Recovery: What the Practitioner Needs to Know and Do. He advocates the inclusion of active symptom and psycho-social management from the day of diagnosis and onward throughout the course of cancer treatment, not solely at the end-of-life.
He currently visits cancer centers around the country for accreditation by the American College of Surgeons Commission on Cancer, and is a volunteer primary care physician at the Coachella Valley Volunteers in Medicine in Indio, California, a program to provide basic healthcare to the under-insured.
During Dr. Fleishman’s tenure as President of APOS (then called ASPBOA), the organization changed from a physician-led group to one with true multidisciplinary membership.
Dr. Fleishman is Board Certified in both Psychiatry and Hospice & Palliative Medicine. Prior to attending medical school, Dr. Fleishman taught in the New York City public schools.
 Charles “Bill” Given, PhD
Charles “Bill” Given, PhD
Charles Given is a Professor in the Department of Family Medicine in the College of Human Medicine at Michigan State University. He is the Director of the Research Institute for Health Care Policy at MSU.
Dr. Given has over 35 years of NIH funded research. During this time he conducted multiple community based inception cohort studies beginning with family caregiving and older patients with the diagnoses of cancer. He completed community based multi-site randomized trials of studies of behavioral interventions for the self care management of symptoms and function among cancer patients. For the last 27 years, patients with cancer, and the family members who assist them during and immediately following treatment has been the focus of his research. His current work involves the use of interactive voice response and internet based systems for assessing and managing cancer related symptoms and adherence for patients taking oral oncolytics. He has been awarded grants from multiple institutes of the NIH including: NINR, NIA, NIMH, NCI, as well as state funds and a grant from the American Cancer Society. Each of these interdisciplinary investigations have been conducted at multiple community based sites, as well as at comprehensive cancer centers. Publications number over 220 papers and 40 book chapters.
Dr. Given was among the 2007 recipients of the CHM Mentor Awards. Selected honors include: BCBSM Foundation Excellence in Research Award in 2001 and 2002; Michael K. Guest Award for Innovative Research, in 2004; MSU, Distinguished Faculty Award in 1997; MSU, College of Human Medicine, Distinguished Faculty Award in 1996; and Arthur Victor Distinguished Faculty Award for Health Care Delivery in 1996.
 Joel Marcus, PsyD
Joel Marcus, PsyD
Dr. Marcus is a clinical psychologist. He has been actively involved in the field of psychosocial oncology since 2001. His personal mission is to help improve the quality of lives of patients and families impacted by cancer.
 Carolyn Messner, DSW, MSW, OSW-C, BCD, LCSW-R, FAPOS
Carolyn Messner, DSW, MSW, OSW-C, BCD, LCSW-R, FAPOS
Dr. Carolyn Messner, DSW, MSW, OSW-C, BCD, LCSW-R, FAPOS is Director of Education and Training at CancerCare where she pioneered the use of teleconference technology to bring evidence-based, psychosocially sensitive cancer-related information to people living with cancer, cancer survivors and their caregivers. A national and international speaker and author, Dr. Messner’s expertise includes the psychosocial impact of cancer on patients and their caregivers, methods to design patient education interventions, and cancer in the workplace. She is an adjunct lecturer at the Silberman School of Social Work at Hunter College. Dr. Messner is coeditor of the inaugural Handbook of Oncology Social Work: Psychosocial Care for People with Cancer (Oxford University Press, 2015). She is a former president of the Association of Oncology Social Work (AOSW) and serves on the boards of several nonprofit organizations. She is on the editorial boards of: Journal of Psychosocial Oncology, Journal of Cancer Education, The Oncology Nurse, The Journal of Interprofessional Practice, and Conquer Magazine.
Dr. Messner’s many honors include Fellow, American Psychosocial Oncology Society (APOS); Fellow, New York Academy of Medicine; AOSW’s Oncology Social Worker of the Year Award; American Cancer Society’s Oncology Social Work Leadership Award; Hyman J. Weiner Award from the Society for Social Work Leadership in Health Care; and the Individual Award for Creativity in Health Care Practice and Scholarship from the National Academies of Practice (NAP). She is a Senior Fellow and Distinguished Practitioner in Social Work, NAP. Dr. Messner received the degree of Doctor of Social Welfare (DSW) from the City University of New York with a Doctoral Fellowship Award in Social Welfare; and The Ohio State School of Social Work National Doctoral Award. She earned a Master of Social Work (MSW) degree from New York University School of Social Work with a National Institute of Mental Health (NIMH) Fellowship, and her bachelor’s degree in Psychology from Clark University, graduating cum laude, Phi Beta Kappa.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2015
 William Breitbart, MD
William Breitbart, MD
William Breitbart, MD is Chairman, The Jimmie C Holland Chair in Psychiatric Oncology, and Chief of the Psychiatry Service, Department of Psychiatry & Behavioral Sciences, Memorial Sloan-Kettering Cancer Center, New York, NY. Dr. Breitbart is also Attending Psychiatrist, Palliative Medicine Service, Department of Medicine at Memorial Sloan-Kettering Cancer Center and Professor of Clinical Psychiatry at Weill Medical College of Cornell University.Dr. Breitbart received the 2003 Research Award from the Academy of Psychosomatic Medicine, the 2007 Donald Oken Award from the American Psychosomatics Society, and the 2008 Lifetime Achievement Award from the Society for Liaison Psychiatry. He is the 2009 recipient of the Arthur Sutherland Lifetime Achievement Award for the International Psycho-oncology Society, and the 2009 recipient of the Willet F. Whitmore Award for Clinical Excellence, Memorial Sloan-Kettering Cancer Center. Dr. Breitbart was the 2011 recipient of the Thomas Hackett Award for Lifetime Achievement from the Academy of Psychosomatic Medicine, and the 2013 recipient of the Jimmie Holland Award from the American Psychosocial Oncology Society. Dr Breitbart is a Past President of the Academy of Psychosomatic Medicine, as well as the International Psycho-oncology Society.
Dr. Breitbart's research efforts have focused on psychiatric aspects of cancer and palliative care. He has had continuous NIH RO1 funding of investigator initiated research since 1989. His most recent efforts have focused on Meaning-Centered Psychotherapy for cancer patients. Dr. Breitbart has published extensively on his clinical research efforts, with over 320 peer review publications, chapters and review papers. In addition, Dr. Breitbart has edited/written 10 textbooks including: Psycho-oncology - 1st , 2nd and 3rd Editions(co-editor with Dr. Jimmie Holland); and treatment manuals on Meaning-Centered Group Psychotherapy in Advanced Cancer Patients, and Individual Meaning-Centered Psychotherapy for Advanced Cancer Patient. Dr. Breitbart is Editor-in-Chief, of Cambridge University Press’ international palliative care journal entitled, “Palliative & Supportive Care”. He helped establish IPOS Press.
 Teresa L. Deshields, PhD
Teresa L. Deshields, PhD
Teresa L. Deshields, Ph.D. is a licensed clinical psychologist and the manager of the Siteman Counseling Service for the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, Missouri. She is also a Clinical Associate Professor in the Department of Medicine at the School of Medicine. She has worked at the Siteman Cancer Center since February, 1999. Her clinical practice is devoted to treating cancer patients and survivors and their family members, throughout the cancer continuum – diagnosis, treatment, survivorship, end of life, grief. Her research is focused on issues related to psychological adjustment and quality of life in cancer patients and survivors.
 Mitch Golant, PhD
Mitch Golant, PhD
Mitch Golant, PhD is a health psychologist and currently Senior Consultant, Strategic Initiatives for the Cancer Support Community (CSC). From 1996 thru 2012 he was CSC’s SVP Research & Training. He has traveled throughout the world introducing CSC’s Patient Empowerment Model to international thought-leaders and psychosocial oncologists. He has been with CSC for over 30 years where he supervised and trained CSC’s professional clinical staff. He has facilitated over 7,000 support groups for people with cancer and trained over 450 professionals nationally and internationally in CSC's Patient Active Support Group model. Dr. Golant is widely recognized as a pioneer in the use of information technology in cancer education and support through the delivery of online support groups. He was central to the launch of the award-winning Cancer Support Community Online in both English and Spanish and Group Loop: Teens. Talk. Cancer. Online. In 2008, he conceived and helped found CSC’s Cancer Survivorship Research & Training Institute. He has presented globally on CSC’s Patient Empowerment programs and evidence-based research including CancerSupportSourceTM—CSC’s distress screening program—and Open to OptionsTM—CSC’s decision support counseling program. He has previously served on the Board of Directors for the American Psychosocial Oncology Society. In October 2011, he received the Los Angeles County Psychological Association’s Distinguished Contribution to the Profession of Psychology Award. He is the contributing editor to the Psycho-Oncology: A Quick Reference on the Psychosocial Dimensions of Cancer Symptom Management, (2006, 2nd Edition, 2014) and The Psychiatric and Psychological Dimensions of Pediatric Cancer Symptom Management (2008 & 2nd Edition, 2014). He is also the co-author of seven books including Reclaiming Your Life After Diagnosis: The Cancer Support Community Handbook (BenBella 2007 revised 2012), What To Do When Someone You Love is Depressed (Holt—updated and expanded 2007), and a contributing author of Psycho-Oncology, 2nd Edition & 3rd Edition (Oxford University Press 2010, 2014).
 William Pirl, MD, MPH
William Pirl, MD, MPH
Dr. William Pirl is Director of the Center for Psychiatric Oncology and Behavioral Sciences at the Massachusetts General Hospital Cancer Center; Associate Professor of Psychiatry at Harvard Medical School, and Associate Director of the MGH Cancer Outcomes Research Program. He is the Past-President of the American Psychosocial Oncology Society. He received his MD from Harvard Medical School and his MPH from the Harvard School of Public Health.
 Kevin Stein, PhD
Kevin Stein, PhD
Dr. Kevin Stein is the Vice President of Behavioral Research for the American Cancer Society (ACS) and the Director of the ACS Behavioral Research Center (BRC), located in Atlanta, GA. The BRC was established in 1995 and conducts original behavioral research to reduce cancer disparities, modify cancer risk behaviors, and improve cancer outcomes and quality of life among cancer patients, survivors, caregivers, and the general population. BRC research informs the development and implementation of evidence-based interventions that directly address quality of life and health behaviors. Our staff also provides behavioral expertise to ACS programs, services, and strategic activities.
Prior to becoming Vice President of Behavioral Research and taking over direction of the BRC, Dr. Stein was Director of Survivorship and Quality of Life Research at ACS. The goals of Dr. Stein’s research are to (a) gain a better understanding of factors related to the physical and psychosocial functioning of persons affected by cancer and (b) develop, test, and disseminate evidence-based interventions to address these issues. He is the Principal Investigator of the American Cancer Society’s Study of Cancer Survivors, a large-scale, nationwide, population-based longitudinal study of quality of life among cancer survivors in the United States. Dr. Stein is the author of over 70 peer reviewed publications and several book chapters. His work has been published in scientific journals and presented at national and international conferences. Dr. Stein’s research has been funded by agencies such as the National Institutes of Health (NIH), Agency for Healthcare Research and Quality (ARHQ), the Centers for Disease Control and Prevention, (CDC), and the Patient Centered Outcomes Research Institute (PCORI).
Dr. Stein received a bachelor’s degree in Psychology from the University of Florida and Master’s and Doctoral degrees in Clinical Psychology from the University of South Florida. He completed an APA-approved internship at the James A. Haley Veterans’ Hospital in Tampa, Florida. Before coming to the American Cancer Society, Dr. Stein completed a three-year Postdoctoral Research Fellowship in Psychosocial Oncology at the Moffitt Cancer Center and Research Institute in Tampa, Florida.
In addition to his work at the American Cancer Society, Dr. Stein is also an Associate Professor (Adjunct) in the Behavioral Sciences and Health Education Department of Emory University’s Rollins School of Public Health. Dr. Stein is an active member of the International Psychosocial Oncology Society, American Psychosocial Oncology Society, The International Society of Quality of Life Research, and the Society of Behavioral Medicine. He is a Fellow of the American Psychosocial Oncology Society, a licensed psychologist in the state of Georgia, and a member of the Georgia Psychological Association.
 Brad Zebrack, PhD, MSW, MPH
Brad Zebrack, PhD, MSW, MPH
Dr. Brad Zebrack is Professor, University of Michigan School of Social Work, and member of the University of Michigan Comprehensive Cancer Center, Socio-Behavioral Program. Dr. Zebrack has clinical social work experience in both pediatric and adult oncology, and has been involved in the development of peer support/advocacy programs for adolescent and young adult cancer survivors. He has published broadly in the fields of medicine/oncology, nursing, psychology, and social work, and serves on the editorial boards for several cancer-related multi-disciplinary peer-reviewed journals. He was a recipient of the Outstanding Education and Training Award from the American Psychosocial Oncology Society (2014) and the Oncology Social Work Research Award from the Association of Oncology Social Work (2002).
Dr. Zebrack’s teaching and research interests are in the areas of health, medicine, cancer survivorship, and quality of life. He is particularly interested in the effects of cancer on the psychosocial growth and development of adolescents and young adults. Over the past 20 years, Dr. Zebrack has been an investigator on numerous research and training initiatives funded by the United States Department of Health and Human Services National Cancer Institute (K07, R03, T32 NRSA, R25), the American Cancer Society, the Lymphoma Research Foundation, LiveStrong Foundation, and HopeLab, Inc.
Dr. Zebrack is a long-term survivor of Hodgkin’s lymphoma, diagnosed in 1985 at the age of 25. In 1989, Brad and his wife Joanne completed a one-year 11,000 mile bicycle trip around the United States to promote cancer survivorship.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Class of 2014
 Mark Lazenby, PhD, MSN
Mark Lazenby, PhD, MSN
Trained as a philosopher of religion, Mark Lazenby left his career as a professional philosopher to earn an MSN in oncology nursing from Yale in 2009. After his MSN, Dr. Lazenby went to the King Hussein Cancer Center in Amman, Jordan, on a Fulbright Scholarship, where he and his colleagues studied the role of religion and spirituality in the well-being of Muslim patients with cancer. He continues to work on issues of spiritual well-being among Muslim patients with cancer. In addition, Dr. Lazenby has studied influences on place of death (home or hospital) in Botswana, Southern Africa, die (home or hospital). His is the first place-of-death study in sub-Saharan Africa. He has also studied the psychological and physical symptoms of patients with cancer in Gaborone, Botswana. Assistant Professor of Nursing and Divinity and Core Faculty on the Council of Middle East Studies at Yale University, he is a co-investigator on the Screening for Psychosocial Distress Program, an NCI-funded program to train cancer care professionals on how to implement and maintain comprehensive distress screening programs. He has served on the APOS Board of Directors since 2012.
 Dr. William Redd
Dr. William Redd
For more than 30 years Dr. William Redd has been a leader in the field of psycho-oncology, beginning with his seminal work on the analysis and control of conditioned aversions in chemotherapy patients. He was among the first investigators to identify the role of behavioral factors in cancer prevention and control. He maintains an active research program and currently has NCI funding to investigate interventions to treat cancer-related fatigue and the dissemination of evidence-based interventions to frontline clinicians. Dr. Redd is credited with mentoring many of the current leaders in the field. He continues his commitment to training the next generation of clinicians and researchers by overseeing national training workshops and by heading a highly successful NCI-funded post-doctoral training program. He credits his bedside interactions with patients as a critical source of hypotheses and intervention strategies.
 Julia H. Rowland, PhD
Julia H. Rowland, PhD
Dr. Rowland is the Director of the National Cancer Institute’s Office of Cancer Survivorship and a long-time clinician, researcher and teacher in the area of psychosocial aspects of cancer. She has worked with and conducted competitively-funded research among both pediatric and adult cancer survivors and their families This work has included a special focus on and a number of studies conducted among breast cancer survivors. She has published broadly in the field of psycho-oncology, serving as co-editor with Dr. Jimmie Holland of the ground-breaking text, Handbook of Psychooncology: Psychological Care of the Patient with Cancer, as well as the Handbook of Cancer Control and Behavioral Science (Miller, Bowen, Croyle, Rowland, eds.). Dr. Rowland is a frequent speaker to both lay and professional audiences on issues related to the long-term and late effects of surviving cancer and has taken an active role in mentoring the next generation of survivorship-focused researchers and clinicians across her career.
Dr. Rowland received her PhD in Developmental Psychology from Columbia University and completed a post-doctoral fellowship at Memorial Sloan Kettering Cancer Center (MSKCC) in psychosocial oncology. While at MSKCC, where she held joint appointments in pediatrics and neurology, Dr. Rowland helped to develop and was the first Director of the Post-Treatment Resource Program (now known as the Resources for Life after Cancer Program), an innovative resource that continues to provide a full range of non-medical services to patients and their families after the end of treatment. In 1990 Dr. Rowland became founding Director of the Psycho-Oncology Program at Georgetown University and the Lombardi Cancer Center in Washington, DC. As part of her work at Georgetown, Dr. Rowland created an innovative program to bring attention to the unique challenges of cancer survivorship. The program paired first year medical students with cancer survivors in active treatment who in turn served as their guides to the art and science of living with, through and beyond cancer.
Dr. Rowland is a member of several advisory boards, including that of the National Coalition for Cancer Survivorship and the American Psychosocial Oncology Society. Since joining the NCI in September 1999, Dr. Rowland has expanded the activities and helped promote the visibility of the Office of Cancer Survivorship, and worked with numerous governmental and non-profit partners to advance public awareness about and secure funding for research addressing the health care and quality of life needs of the growing population of cancer survivors and their families. Dr. Rowland’s expertise in and deep commitment to championing this field earned her Fellow status in 2006 within both the American Psychological Association’s Division of Health Psychology and the Society of Behavioral Medicine.
 Lori Wiener, PhD, DCSW
Lori Wiener, PhD, DCSW
Dr. Lori Wiener is co-director of the Behavioral Science Core and head of the Pediatric Psychosocial Support and Research Program in the Pediatric Oncology Branch of the National Cancer Institute (NCI). She has been central to the fields of pediatric psychosocial oncology and pediatric HIV. Her previous affiliations included work with adult cancer patients at Memorial Sloan Kettering Cancer Center and as a pioneer in the early AIDS epidemic, running the first support groups for persons living with what was then referred to as Gay Related Immune Disease (GRID) and AIDS Related Complex (ARC). In 1986, Dr. Wiener joined NCI's pediatric oncology branch where she developed a robust clinical and research program that has focused on critical clinical issues that had not previously been studied in the HIV field, including parental needs and coping, children's distress, father's experiences, sibling issues, diagnosis disclosure, and loss and bereavement and later, with pediatric oncology families, studying areas such as lone parenting, transnational parenting, emotional consequences of medically required isolation, sibling donor experiences, graph versus host disease, and end-of-life planning. She currently is the Principal Investigator on 10 psychosocial studies. Dr. Wiener has also dedicated a substantial part of her career to applying knowledge from her clinical experience and psychosocial studies to create innovative resources such as workbooks, games and Voicing My Choices, an advance care planning guide for adolescents and young adults. Dr. Wiener is the senior editor of a Reference for Pediatric Oncology Clinicians: The Psychiatric and Psychological Dimensions of Pediatric Cancer Symptom Management, available through the American Psychosocial Oncology Society.
 James Zabora, SCD, MSW
James Zabora, SCD, MSW
Dr. James Zabora came to the position of Director of the Life with Cancer Program for the Inova Health System in Northern Virginia after serving as Dean and Professor of Social Work at the National Catholic School of Social Service (NCSSS) of The Catholic University of America (CUA) for 10 years. Prior to CUA, Dr. Zabora had a 20 year career at The Johns Hopkins University School of Medicine. As an administrator, he served as one of the five Associate Directors in the Comprehensive Cancer Center with a special focus on community programs and research. Along with Mr. Matthew Loscalzo, Dr. Zabora developed what was considered to be the best psychosocial services for cancer patients and their families in the United States. Currently, Dr. Zabora’s research continues to focus on cancer prevention and control, psychosocial screening, problem-solving education, and quality of life among cancer patients and their families.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Inaugural Class of 2013
 Terry Badger, PhD, PMHCNS-BC, RN, FAAN
Terry Badger, PhD, PMHCNS-BC, RN, FAAN
Dr. Badger is Professor and Director of the Community and Systems Health Science Division at The University of Arizona College of Nursing, Professor in the Department of Psychiatry, and member of The University of Arizona Cancer Center. Her research is in the area of psychological distress, dyadic interdependence between emotional states of breast and prostate cancer survivors and members of their social network, and telephone psychosocial interventions. She is the current Past-President of APOS.
 Wayne A Bardwell, PhD, MBA
Wayne A Bardwell, PhD, MBA
Dr. Bardwell is Associate Professor of Psychiatry in the University of California San Diego School of Medicine, and Director of the Patient and Family Support Service and the Doris A. Howell Palliative Care Service at the Moores UCSD Cancer Center. Dr. Bardwell’s research focuses on understanding links between physiological and psychosocial (depression, fatigue, sleep) functioning in chronic medical illness (breast cancer, obstructive sleep apnea). Dr. Bardwell’s clinical experience has included conducting individual and group psychotherapy for adult inpatients and outpatients with chronic and life-threatening medical illnesses (including breast and other cancers, spinal cord injury, chronic pain, HIV/AIDS).
 Donna B Greenberg, MD
Donna B Greenberg, MD
Dr. Greenberg is Director, Psychiatric Oncology Service at the Massachusetts General Hospital. Her specialties include psychiatric oncology and behavioral sciences and neuro-oncology. Dr. Greenberg is a past president and treasurer of APOS, as well as the 2008 Conference Chair. Dr. Greenberg has been an active supporter of APOS since its inception.
 Jimmie C Holland, MD
Jimmie C Holland, MD
Dr. Holland, recognized internationally as the founder of the subspecialty of psycho-oncology, is Attending Psychiatrist and holds the first endowed chair in Psychiatric Oncology, the Wayne E. Chapman Chair at Memorial Sloan-Kettering Cancer Center. She is Professor of Psychiatry at Weill Medical College of Cornell University. She began the first full-time Psychiatric Service in a cancer hospital in 1977 at Memorial Sloan-Kettering Cancer Center, and in 1996, she became the first woman Chair of a clinical department at Memorial. From this base, the concept of psycho-oncology evolved to become a nationally recognized subspecialty of oncology. The Department of Psychiatry & Behavioral Sciences has trained over 300 psychologists and psychiatrists in both clinical and research areas. Dr. Holland was PI of the first research training grant in psycho-oncology, which has continued uninterrupted for 29 years. Dr. Holland studied the prevalence and nature of psychological problems in patients with cancer in the 1970s and established the first committee studying psychological and quality of life issues in a cooperative group, the Cancer Leukemia Group B. In the 1980s she became the Founding President of the International Psycho-Oncology Society (1984) and of APOS (1986).
 Paul B Jacobsen, PhD
Paul B Jacobsen, PhD
Dr. Jacobsen is Associate Center Director for Population Science at Moffitt and Professor of Psychology and Oncologic Sciences at the University of South Florida. For the past 25 years, his work has focused on using knowledge from the behavioral and social sciences to promote reductions in cancer risk, early detection of cancer, and improvements in quality of life following cancer diagnosis. Dr. Jacobsen is the author of more than 200 journal articles and the recipient of numerous research and training grants from the American Cancer Society and the National Cancer Institute. In 2008 he received the Bernard Fox Memorial Award for outstanding contributions to psychosocial oncology from the International Psycho-Oncology Society, and in 2010 he received the Holland Distinguished Leadership Award from the APOS. He is a past president of APOS and is closely involved in the society’s efforts to develop and promote quality standards for psychosocial care of cancer patients.
 Matthew J Loscalzo, LCSW
Matthew J Loscalzo, LCSW
Professor Loscalzo is the Liliane Elkins Professor in Supportive Care Programs in the Department of Supportive Care Medicine and Professor in Department of Population Sciences. He is also the Executive Director of the Department of Supportive Care Medicine and the Administrative Director of the Sheri & Les Biller Patient and Family Resource Center at the City of Hope-National Medical Center, Duarte California. Professor Loscalzo has over 30 years experience in caring for cancer patients and their families. He is recognized internationally as a pioneer in the clinical, educational, and research domains of psychosocial aspects of cancer. Professor Loscalzo is a past president of APOS and the Association of Oncology Social Workers. His areas of focus have been pain and palliative care, the implementation of problem-based screening programs, gender-based medicine and problem solving therapies.
 Ruth McCorkle, PhD, FAAN
Ruth McCorkle, PhD, FAAN
Dr. McCorkle is the Florence S. Wald Professor of Nursing at the Yale School of Nursing, Professor of Epidemiology, and was Program Leader of Cancer Control at the Yale Comprehensive Cancer Center from 1998 to 2010 and was recently appointed Assistant Director of Psychosocial Oncology Research. An international leader in cancer nursing, education and cancer control research, Dr. McCorkle has done landmark research on the psychosocial ramifications of cancer. Dr. McCorkle has had continuous funding from the National Institutes of Health since 1983. Currently, she is the principle investigator of “An Intervention to Improve Outcomes in patients with Advanced Cancer,” a grant funded by the National Institute of Nursing Research. She was awarded the first biomedical institutional training grant from the National Cancer Institute in Psychosocial Oncology at the University of Washington in 1983. Subsequently she has been the program director on institutional training grants at both University of Pennsylvania and is currently the co-director at Yale University. Dr. McCorkle joined the faculty of the Yale School of Nursing in 1998 to assume a leadership of the institution’s doctoral program and was the founding Director of the Center for Excellence in Chronic Illness.
 Peter Trask PhD, MPH
Peter Trask PhD, MPH
Dr. Trask received his doctorate in Clinical Psychology from the University of Maine in 1997. Dr. Trask then engaged in a two-year postdoctoral fellowship in Behavioral Medicine at the University of Michigan where he began a research program focused on assessing and treating emotional distress and changes in quality of life in individuals diagnosed with cancer. His research studies focused on a variety of cancer diagnoses and treatments. He continued this research, and provided therapy to cancer patients, during the subsequent four years that he was a faculty member in the Department of Psychiatry at the University of Michigan. In 2003, Dr. Trask became Assistant Professor of Research at Brown University in the Centers for Behavioral and Preventive Medicine. For six years, Dr. Trask was employed in the Outcomes Research group in the Oncology Business Unit at Pfizer. He was responsible for developing strategies for assessing health economic and patient-reported outcomes for multiple early and late phase oncology compounds. He has continued this work as Director in Oncology in the Global Evidence and Value Development group at Sanofi. Dr. Trask is a past recipient of the APOS New Investigator award, a past Treasurer and President of APOS, and continues to give back to the organization he has been a part of since 2003 as part of the Membership Committee.
 Alan Valentine, MD
Alan Valentine, MD
Dr. Valentine is Professor and Chair, Department of Psychiatry, the University of Texas MD Anderson Cancer Center. He served as APOS President in 2004 and was the recipient of the 2009 Holland Distinguished Leadership Award.
 Deane L Wolcott, MD
Deane L Wolcott, MD
Dr. Wolcott is a psychiatrist who has spent most of his professional life leading and supporting the development of supportive care services in the hospital cancer program environment. He is currently Director of Oncology Supportive Care Services at the Samuel Oschin Comprehensive Cancer Institute at Cedars-Sinai Medical Center in Los Angeles. He has been an active member of APOS since its inception and is a past president of APOS. He has also been a member of the Professional Advisory Board of the Cancer Support Community. He has served as Program Chair for the 2013 APOS 10th Annual Conference. Dr. Wolcott is strongly committed to the multidisciplinary team model of oncology supportive care services.

